How Stool Habits Reveal Clues About Mental Health
Have you ever wondered why you or your child are more anxious, irritable, or emotional when digestion is off? Or why constipation or diarrhea always seem to come with sleep issues or meltdowns? That’s not just coincidence — it’s the gut-brain connection at work.
Our gut is often called the “second brain” for a reason. Through nerves, neurotransmitters, and even the bacteria in our intestines, the gut sends constant messages to the brain — impacting mood, behavior, focus, and even emotional resilience. And one of the easiest ways to assess gut health? Pay attention to stool habits and appearances.
The gut and brain are in constant communication through a bi-directional pathway known as the gut-brain axis. At the center of this is the vagus nerve—the longest nerve in your body that runs from your brainstem down to your digestive organs.
Think of the vagus nerve as the body’s information superhighway:
It sends signals from your brain to your gut to regulate digestion.
It sends signals back from your gut to your brain—reporting on inflammation, microbial balance, and nutrient status.
Around 70-80% of vagus nerve signals go from gut → brain, not the other way around.
This is one reason why digestive dysfunction can show up as anxiety, irritability, foggy thinking, or behavior issues—especially in children with sensitive nervous systems.
What Stool Habits Can Tell You About the Gut-Brain Connection
Let’s break it down:
Constipation
When stool stays in the colon too long, toxins and hormones can be reabsorbed, which may increase irritability, anxiety, or mood swings. It’s especially common in overstressed women or sensory-sensitive children.
Loose Stools / Diarrhea
Often a sign of inflammation, infection, or nervous system dysregulation (fight-or-flight mode). Some kids or adults with anxiety have “nervous tummy” that shows up as urgent BMs.
Undigested Food
May indicate low stomach acid or enzyme function, which can reduce nutrient absorption—key for brain health and neurotransmitter production.
Strong Odor or Excessive Gas
Can signal imbalances in gut bacteria, which may contribute to brain fog, meltdowns, sleep disturbances or even skin health (eczema, acne, etc.)
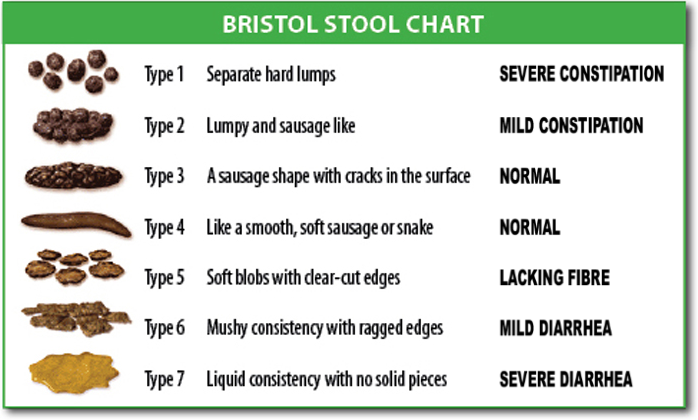
The Bristol stool scale is a tool developed in 1997 to classify the way feces looks into seven different categories.
The ideal stool is Type 3 &4. Types 1 & 2 signifies constipation. Type 5 lacks fiber from the diet, and Types 6 & 7 are signs of diarrhea.
The Microbiome’s Role in Mental Health
Your gut houses trillions of bacteria—some helpful, some not. This microbial community is responsible for producing mood altering neurotransmitters like serotonin, dopamine, and GABA.
When the microbiome is imbalanced (a state called dysbiosis), the brain receives faulty messages. Below are some common imbalances that affect the nervous system:
Yeast Overgrowth (like Candida):
→ Produces toxins (like acetaldehyde) that stress the liver and disrupt the nervous system. Often associated with brain fog, fatigue, sugar cravings, irritability, an increased anxiety in both adults and kids.Parasites:
→ These stealthy invaders can trigger chronic immune activation, poor nutrient absorption, and nervous system “hypervigilance.” Many kids with persistent meltdowns or sensory issues show parasite markers without classic GI symptoms.Opportunistic Bacteria Overgrowth (e.g., Citrobacter, Klebsiella, Clostridia):
→ These bacteria can release neurotoxins and affect neurotransmitter breakdown. For example, Clostridia species can interfere with dopamine conversion, leading to mood swings or rage-like episodes.Leaky Gut / Inflammation:
→ Damage to the gut lining allows inflammatory molecules to enter circulation, crossing the blood-brain barrier and promoting anxiety, irritability, or poor stress tolerance.What Lab Markers Reveal About Mood
I use a comprehensive stool test like the GI MAP in my practice. It reveals more than just infections, it shows patterns that correlate with brain-based symptoms. Here are key markers I look at:
Low Beneficial Bacteria =associated with low resilience, mood instability, and poor gut lining integrity
High Inflammatory Bacteria or Pathogens= H. Pylori, Clostridia, or Staph/Strep overgrowths can drive skin or behavioral symptoms in kids and anxiety in adults
Leaky gut = immune activation, food sensitivities, and anxiety-like symptoms
Yeast overgrowth=mood swings, sugar cravings, fatigue, and skin issues
Secretory IgA (sIgA)=marker of immune defensiveness affecting mood, stress response and pathogen susceptibility
Calprotectin / Anti-Gliadin / Zonulin=markers of gut inflammation, immune reactivity, and permeability (“leaky gut”) all linked to mood disorders and behavioral challenges
Real-Life Symptoms of a Disrupted Gut-Brain Axis
In Kids:
Frequent meltdowns, mood swings, or hyperactivity
Bedtime battles, night waking
Constipation, picky eating, gassiness, itchy anus
eczema, rashes, food sensitivities
In Women:
Anxiety, PMS, depression, or postpartum mood struggles
Brain fog, fatigue, poor stress tolerance
IBS-like symptoms, food sensitivities, or irregular stools
Skin rashes, acne, canker sores
How to Support the Gut-Brain Connection Naturally
1. Feed the Good Bacteria
Include prebiotic-rich foods like bananas, garlic, and cooked/cooled potatoes.
Add fermented foods (if tolerated): yogurt, kefir, sauerkraut, or coconut water kefir.
Be cautious if this worsens gut symptoms. As someone who has had SIBO (small intestinal bacterial overgrowth), that can feed an already overgrown terrain.
2. Regulate the Nervous System
Practice vagus nerve stimulation: humming, gargling, blowing, deep belly breathing.
Incorporate sensory-rich play or movement for kids (swings, bouncing, crawling).
3. Stay Hydrated & Support Regular BMs
Use magnesium-rich foods (avocados, pumpkin seeds) or supplements as needed.
Fiber + hydration = the magic combo.
4. Consider Functional Testing
GI MAP stool testing or nutrient panels can offer insight into microbial balance and inflammation.
Tailored supplementation is always more effective than guessing.
Ready to Go Deeper?
If your mental health or your child’s behavior seems unpredictable, don’t underestimate the role your gut is playing. The stool you flush each day might just be the biggest clue your body is giving you.
You can calm the brain by healing the gut.
If you’ve been trying to piece things together on your own—googling symptoms, eliminating foods, or buying random supplements without real results—you’re not alone. Healing the gut-brain connection takes more than guesswork. Functional testing and a personalized plan with a skilled practitioner can save you time, money, and frustration.
Whether it’s you or your child who’s struggling, healing doesn’t have to be a DIY journey. As a pediatric occupational therapist and functional practitioner, I’ve worked with countless families who had tried everything—yet still felt stuck. For many of these women and children, the missing piece was gut health. When we address root causes like nutrient deficiencies, dysbiosis, and nervous system stress, things begin to shift—mood stabilizes, meltdowns ease, energy returns.
If you're ready for a personalized, root-cause approach that sees the whole picture, I’m here to help.
👉 Book a free consult here: https://my.practicebetter.io/#/65195dc8777369c2977d6c1c/bookings or check out my package details here: https://www.amywiseliving.com